2022 Impact Report
COVID-19: A long road to recovery
Continuing the fight
As we move into the third year of the COVID-19 pandemic, a great deal has changed – but our commitment to supporting patient outcomes and the heroic efforts of our health care workers has not.

Thanks to the development of lifesaving vaccines, the nature of our battle against the virus has evolved, and as a society, system and foundation, we are moving from crisis response to recovery.
The road to recovery
While we hope the darkest days of the pandemic are behind us, we still have a great deal of work ahead. Our hospitals are at capacity meeting the needs of patients who have waited for surgeries, diagnostics and mental health care. Health care workers have stepped up in ways beyond expectation and the last two years have taken their toll on the wellbeing of our devoted caregivers. Finally, the emergence of “Long COVID” and other post-infection complications are going to require significant research, innovation and treatment plans to respond to this new, chronic disease.
Long COVID
Beyond the acute crisis phase of the pandemic, a new challenge has been revealed for COVID-19 patients: Long COVID. From the earliest days of COVID-19, there was anecdotal evidence of post-viral symptoms and abnormalities that hung around long after the initial infection in some people. That evidence has been increasingly studied and a condition known as Long COVID has been identified.
Long COVID manifests itself in many ways and researchers are still working to understand them all. We do know that Long COVID affects a variety of different body systems – sometimes concurrently – in ways that can be tremendously debilitating for patients.
Systems under strain
Early research has discovered a handful of systems hit hard by Long COVID. Any challenge to an individual system is hard enough, but with many Long COVID cases, patients have a combination of challenges that can severely affect their standard of living.

Brain
It’s known colloquially as “brain fog”, a condition some patients describe as cognitive challenges – often forgetting what they were saying midsentence. Researchers have discovered concerning evidence about a lack of oxygen to the brain and a literal reduction in the brain size of many people.
Lungs
Many people suffering from Long COVID often describe difficulty breathing and there’s mounting evidence that shows lung damage even in patients who only experienced a mild initial infection.

Circulatory system
One of the most common symptoms of Long COVID is a general sense of exhaustion and an acute inability to perform simple physical tasks like climbing a set of stairs. Researchers have identified the effects of a COVID-19 infection on the circulatory system as likely being the culprit.
Immune system
Many of the lingering and ongoing symptoms of COVID-19 that Long COVID sufferers complain about are the result of the virus’s effect on the immune system. While the research is ongoing, scientists believe that the virus may damage the immune system and embed itself deeply into tissues, forcing the immune system to continue fighting long after the initial infection has passed.
10-30%
of people Infected with COVID-19 will have Long COVID.
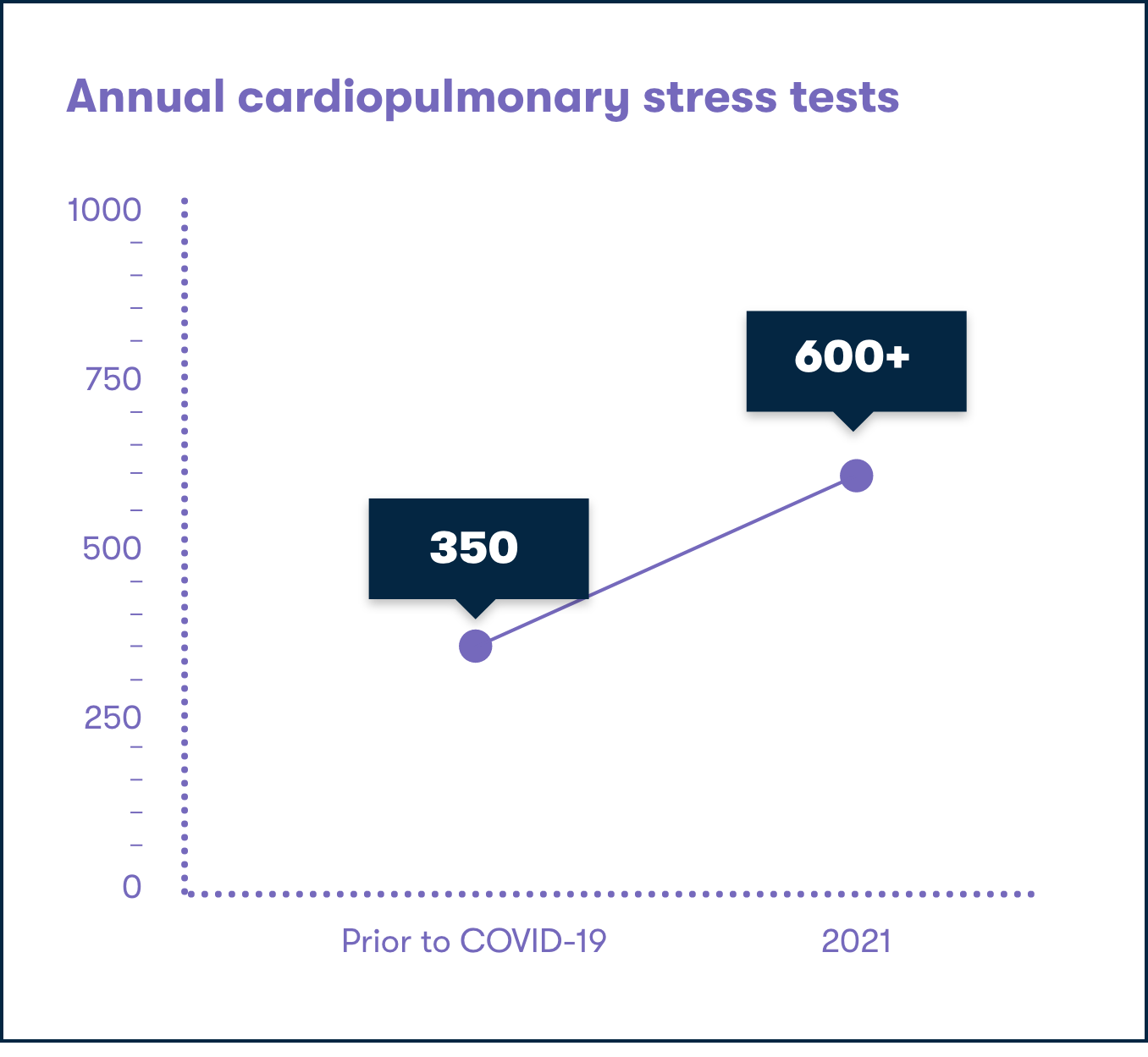
Investing in Long COVID clinics and diagnostic equipment
As we travel the road to recovery, diagnosing and treating Long COVID will become increasingly important for countless Albertans looking for breakthroughs.
To begin providing Long COVID care, AHS has developed two multidisciplinary clinics in Calgary and enhanced Long COVID care through the specialized respiratory clinics at Peter Lougheed Centre and Rockyview General Hospital. At the core of respiratory health diagnostics, research and treatment plans are the important pieces of cutting-edge technology that empower cardiopulmonary stress tests (CPETs). This equipment allows health care teams to identify Long COVID respiratory symptoms and also helps diagnose multiple cardiac and pulmonary diseases.
To help meet the increase in demand from the ongoing pandemic, we are able to help acquire the necessary equipment to provide patients with respiratory tests and information that can help them work towards better outcomes.

Caring for health care workers
Countless lives have been saved and made better over the course of the COVID-19 pandemic by brave and dedicated healthcare workers. But this sustained, challenging work has impacted the mental health of the people we entrust to care for our entire community. Caring for caregivers and rebuilding their resilience is a top priority.
Calgary and surrounding communities care providers
38,126
Staff
3,181
AHS PHYSICIANS
4,918
VOLUNTEERS
a moment of gratitude
It’s impossible to convey the depth of our collective gratitude to everyone in health care, but working with our generous donors we wanted to remind care providers just how much they mean to us. We delivered messages of appreciation and snacks to health care campuses around the city to provide a moment of rest and care.
Spaces to rest, relax and regroup
For patients and staff alike, hospitals and care centres are places of great stress. For countless staff members in Calgary’s hospitals, the demands of these spaces have become more obvious.
Working with AHS, we’ve identified spaces at Foothills Medical Centre, Peter Lougheed Centre, Rockyview General Hospital and South Health Campus to be transformed into tranquil and private areas for health care staff to use to rest and recharge. By renovating existing and underutilized spaces into specially designed areas for health care staff to enjoy on a break, we can not only show our gratitude, but also provide a much-needed boost to their mental health and well-being.

Art therapy: Wait for Me
Art doesn’t just have the power to heal – it has the power to reveal truths that bring us together. Musician and songwriter, Dr. Grant Kennedy, and photographer, Dr. Heather Patterson, collaborated to create a song and video that brought the mental health challenges of the pandemic to the forefront. What makes this even more special is both artists are also Emergency Room physicians. We were excited to collaborate on this production and help empower healing through song, community and open honesty.

